The patient is a woman in her 60’s who self referred for complaint of abdominal pain, weight loss, and rest pain of the lower extremities. She is a 40 pack year smoker and had severe COPD, hypertension, congestive heart failure with mitral regurgitation, chronic kidney disease stage IV, and ischemic rest pain of the legs. She had a 30 pound weight loss due to severe postprandial abdominal pain. She had bloody stools. Her kidney function was worsening, and dialysis was being planned for likely renal failure but she was against dialysis. She had consulted several regional centers but was felt to be too high risk for surgery and with her refusal of dialysis, would be a high risk for renal failure and death with intervention. Physical examination revealed weakened upper extremity pulses, and nonpalpable lower extremity pulses and a tender abdomen. In clinic, she developed hypoxia and dyspnea and was admitted directly to the ICU.

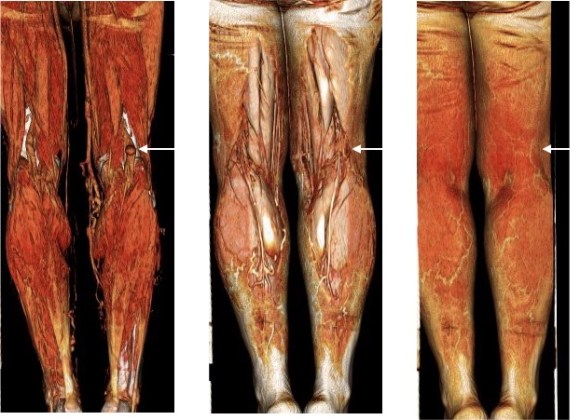
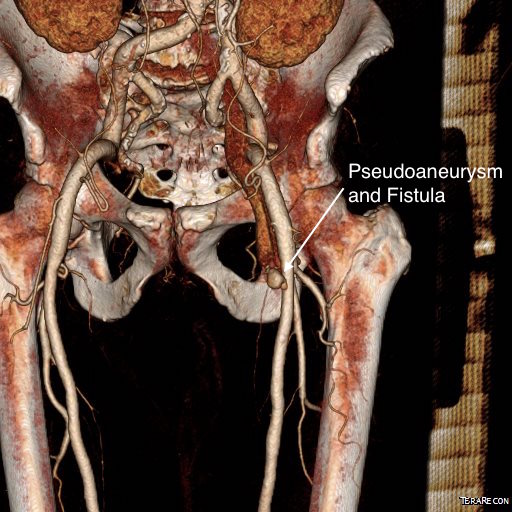
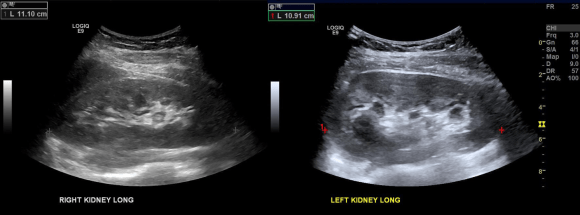
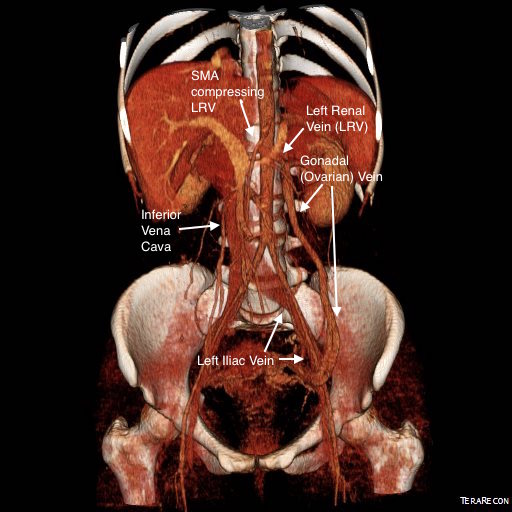
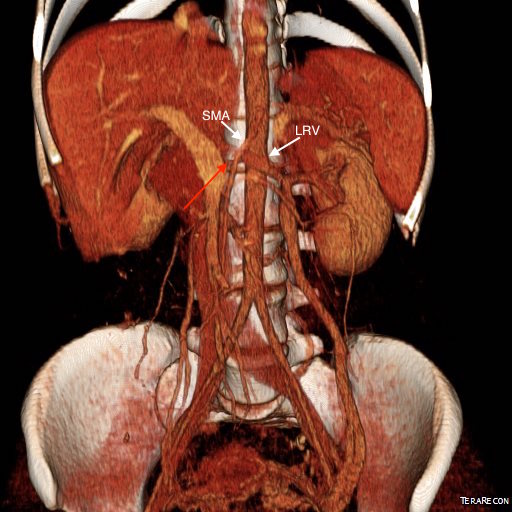
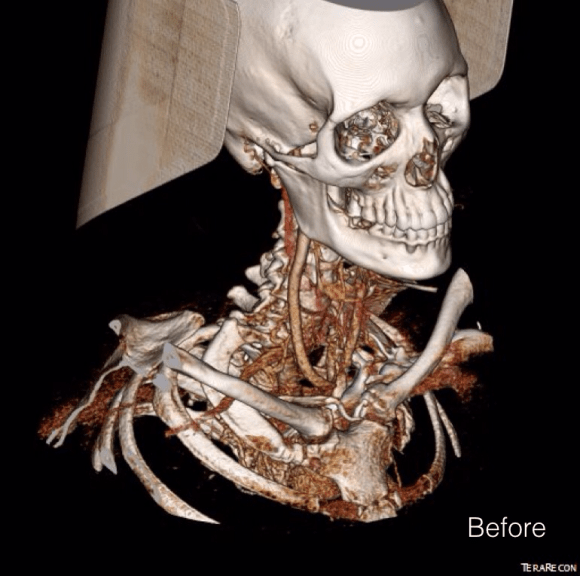
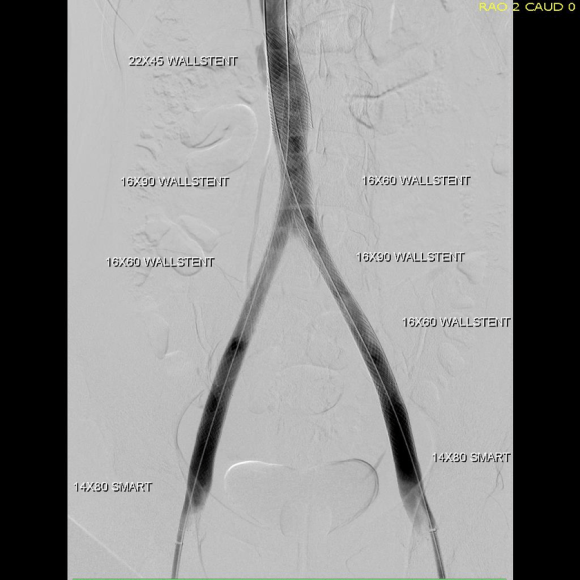
CTA (above) revealed severely calcified atherosclerotic plaque of her visceral segment aorta occluding flow to her mesenteric and renal arteries and to her leg. The right kidney was atrophic. The left kidney had a prior stent which looked crushed. The infrarenal aorta was severely diseased but patent and there were patent aortic and bilateral iliac stents.
Echocardiography revealed a normal ejection fraction of 60%, diastolic failure, +2 to+3 mitral regurgitation, and pulmonary artery hypertension. She did respond to diuresis and stabilized in the ICU. Intervention was planned.
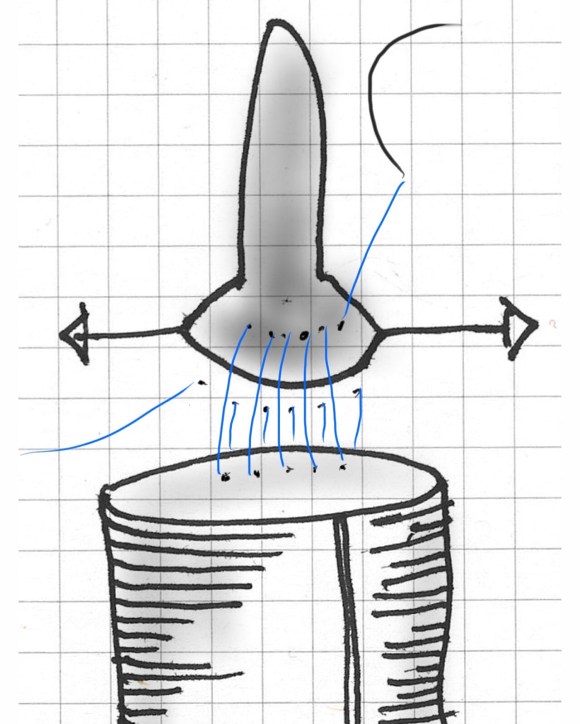
Options that I considered were an extranatomic bypass to her legs and revascularization from below. I have come across reports of axillo-mesenteric bypass, and I have performed ascending and descending thoracic aorta to distal bypass for severe disease, but concluded, as did the outside centers, that she was a formidable operative risk. Also, there was a high likelihood of great vessel occlusive disease. Looking at her CTA, I felt that she needed just a little improvement in flow -not perfect but good enough. The analogy is like drilling an airline through a cave-in. Also, her left kidney gave a clue -it was normal sized and survived the stress test of a contrast bolus for the CTA without dying. A discussion with the patient green lighted an attempt -she understood the cost of failure but did not wish to linger with this abdominal pain.
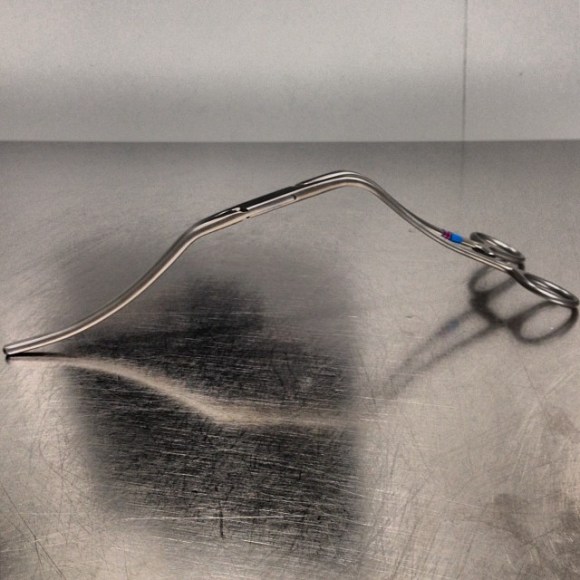
Access for intervention was via the left brachial artery. Aortography showed the severe stenosis at the origin of the SMA and the nearly occlusive plaque in the visceral segment aorta.
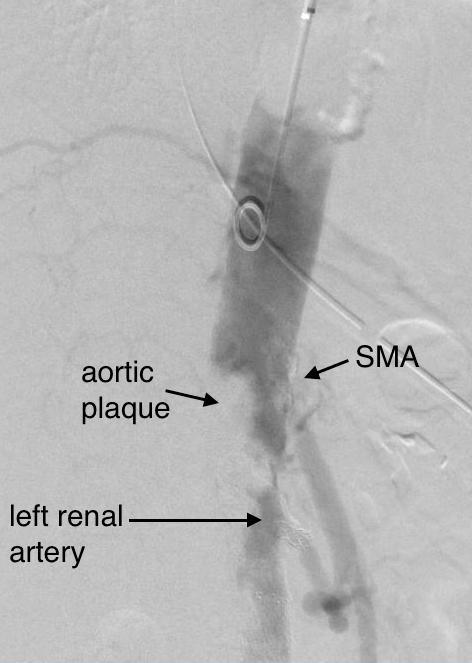
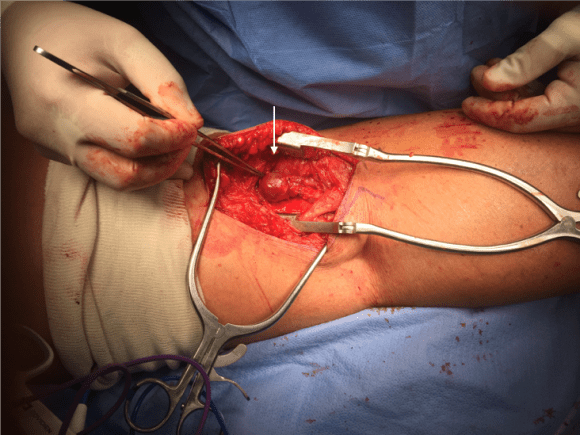
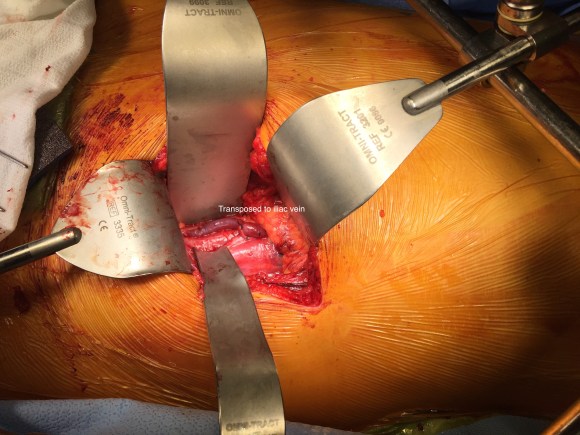
The plaque was typical of the coral reef type, and had an eccentric channel that allowed passage of a Glidewire. Access into the left renal artery was achieved. Its stent was patent but proximally and distally there were stenoses; this was treated with a balloon expandable stent. The path to it was opened with a balloon expandable stent to 8 mm from femoral access. This was the improvement the renal needed. A large nitinol stent was placed from this access in the infrarenal aorta when severe disease above the iliac stents was encountered. The SMA was then accessed and treated with a bare metal stent.

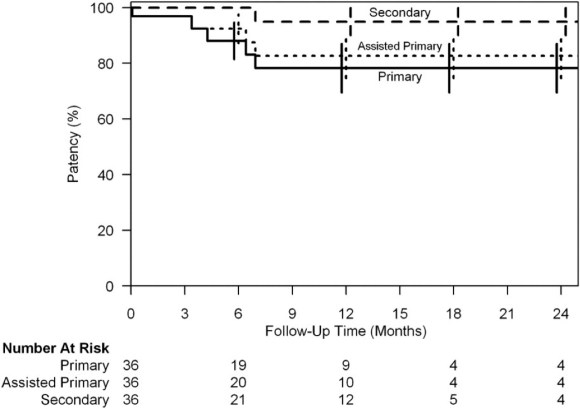
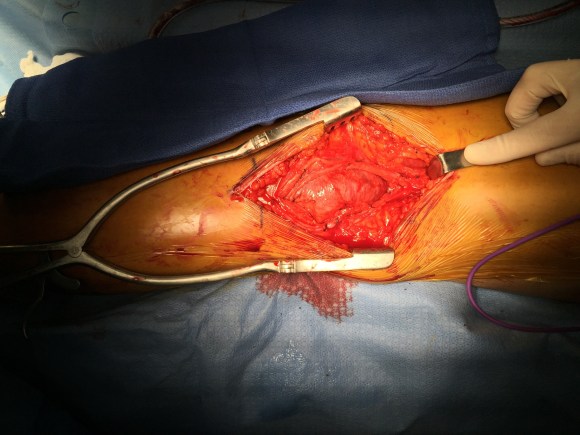
Her creatinine improved, as did her intestinal angina. She was discharged home. She later returned a month after the procedure with complaints of nausea and vomiting and right lower quadrant abdominal pain and was discovered to have an ischemic stricture of her small bowel. This was removed laparoscopically and she recovered well. She recovered her lost weight and now a year and a half later, remains patent and symptom free.
Discussion: Dr. Jack Wiley includes in the preface to his atlas of vascular surgery the words of Dr. Joao Cid Dos Santos, the pioneer of endarterectomy techniques, “Vascular surgery is the surgery of ruins.” And in that context, good enough is sufficient.

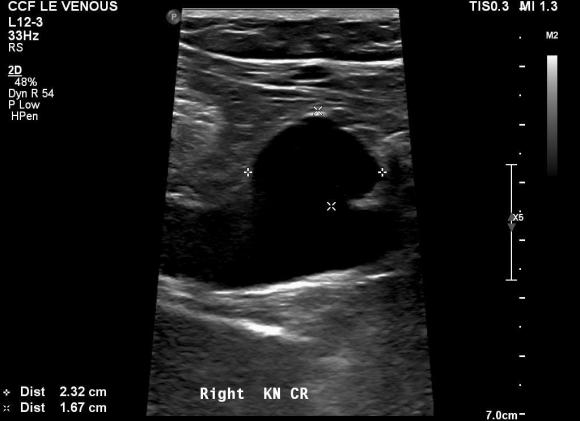
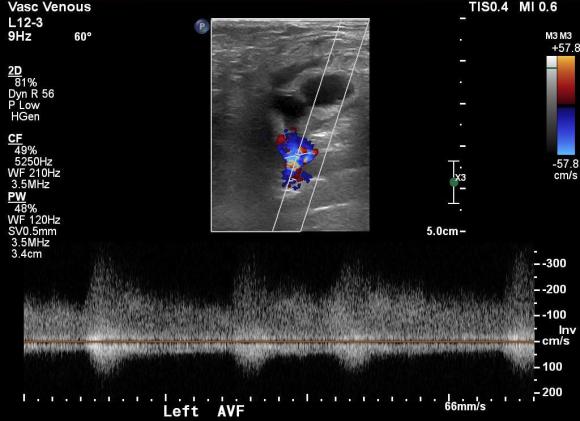
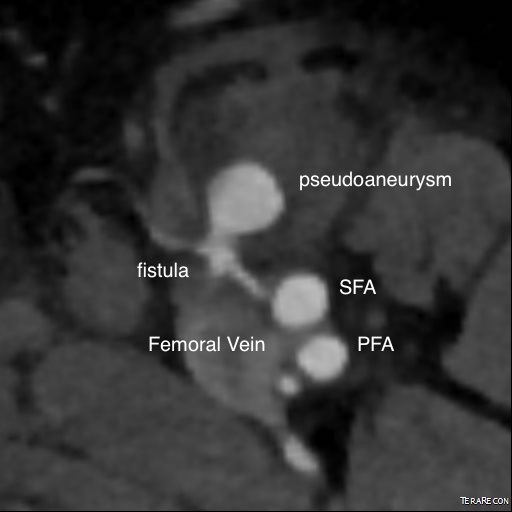
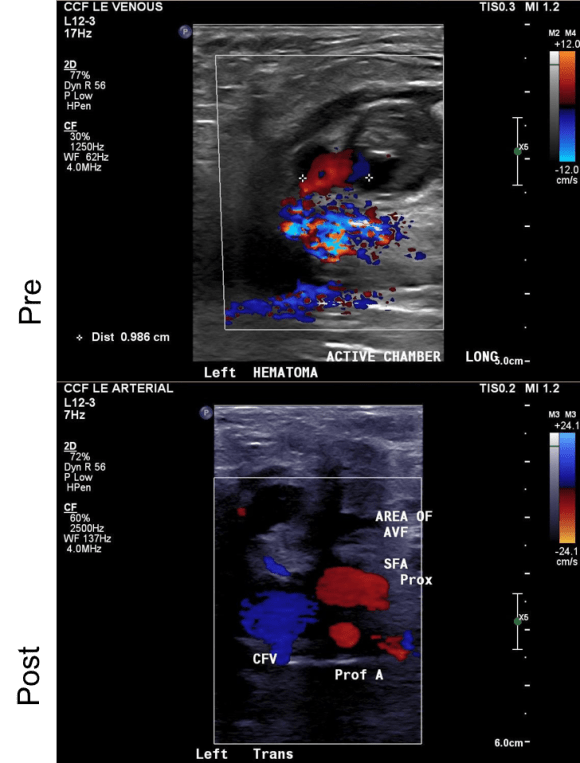
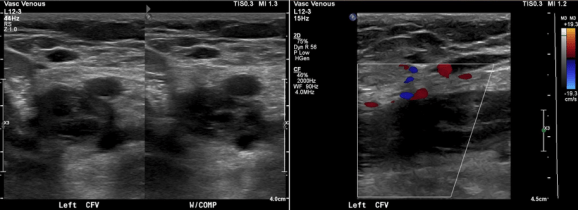 The patient is a young woman who three weeks prior to presentation developed sudden low back pain and left leg pain while exercising on an elliptical. This pain worsened through the subsequent weeks and she developed fevers, chills, and night sweats, and she came to the emergency department. There, she was found to have left thigh and leg swelling. Duplex revealed a left iliofemoral DVT starting from the iliocaval tributary and extending to her left femoral vein (figure above). A CT scan revealed a pulmonary embolism to the left lung (below). No precipitating factors were present. Vascular surgery was consulted.
The patient is a young woman who three weeks prior to presentation developed sudden low back pain and left leg pain while exercising on an elliptical. This pain worsened through the subsequent weeks and she developed fevers, chills, and night sweats, and she came to the emergency department. There, she was found to have left thigh and leg swelling. Duplex revealed a left iliofemoral DVT starting from the iliocaval tributary and extending to her left femoral vein (figure above). A CT scan revealed a pulmonary embolism to the left lung (below). No precipitating factors were present. Vascular surgery was consulted.