The patient had been suffering with dysphagia for over a decade and had had extensive head and neck work up which found a goiter. Medical treatment of this goiter failed to relieve the lingering sensation of food getting stuck and the constant feelingof choking. It was only after a search for mediastinal sources of dysphagia that an aberrant right subclavian artery was found.

One of the advantages of working at the Clinics (I was a fellow at the Mayo, and currently on staff the the Cleveland) is that the infrequent is common while the common is rare. Recently in clinic, I had not one but two patients with dysphagia lusoria. It was the observation of Dan Clair’s, chairman emeritus, that by simply transposing the aberrant and yet nonaneurysmal right subclavian artery, the tension on the esophagus and trachea are relieved. Or as the dictum might go: it takes two hands to garrote someone.

The question is then what to do with the stump? The natural history of the untreated stump is unknown but may be more benign than one might assume. It certainly doesn’t degenerate into an aneurysm all the time -chest CT’s are fairly common and when these are discovered, they are not usually aneurysmal like persistent sciatic arteries which present typically as aneurysms with thromboembolism. Perhaps because we don’t sit on the subclavian artery as we would on a persistent sciatic artery that these aberrant right subclavian arteries don’t degenerate.

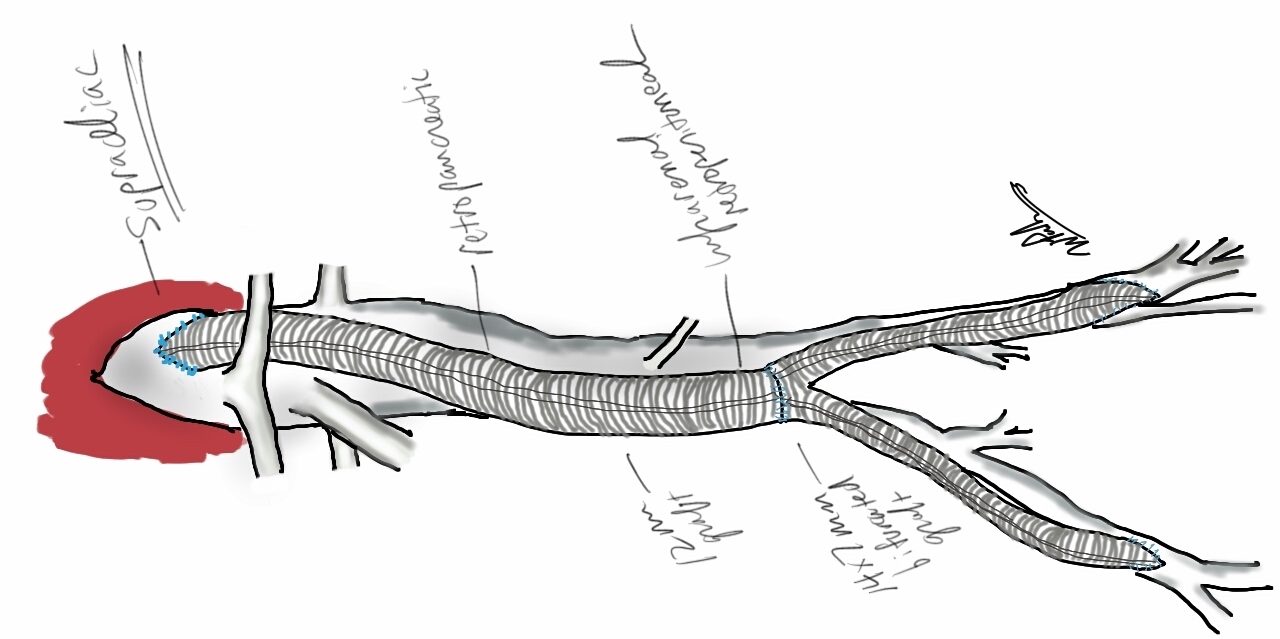
The old fashioned way I learned to treat these aneurysms (Kommerell Diverticula) was through a high thoracotomy and short graft repair of the aorta, replacing the origin of the diverticulum. This is a dangerous operation for an older, sicker, and often cachectic patient. The more recent reports involve a left carotid subclavian bypass or transposition and TEVAR after a right carotid subclavian revascularization. This second step may be unecessary if the non-aneurysmal stump proves to be benign. I don’t recommend coil embolization of the stump as mass effect of packed coils adjacent to the esophagus can cause dysphagia to recur, and this may necessitate an open resection and repair (observation, DC).
The patient underwent a successful right carotid subclavian transposition and had immediate relief of her dysphagia for the first time in over a decade, especially because she had been told she may have been imagining the discomfort. Kudos to her physicians who ordered the CT of the chest that discovered her arch anomaly. Follow up at 6 weeks showed a stable subclavian stump and patent transposition (images above). My plan is for regular interval CT’s with increasing intervals as time passes.