Percutaneous access for EVAR and TEVAR does several things. First, the procedure becomes shorter by an hour or two, and (don’t discount not having nursing count instruments because the case was percutaneous). Second, the patients experience far less discomfort and it is easier to discharge them the next day when they have a bandaid versus an incision. And this leads to the third thing: not having an incision means it is far less likely that a groin infection will occur, especially in the obese.
There are three things which you must do before undertaking pEVAR. First, you have to become comfortable with using the Perclose S device in 6F-8F access -about 5 to 10 successful closures will do. You should become facile with the deployment of the sutures and closure of the access point. Avoid small arteries or heavily calcified arteries. This leads to the second point -all of your groin access should be ultrasound guided -this has been shown to improve results in pEVAR (Ref 1). I am a firm believer that the source of groin access complications starts with the initial needle stick. The 18g needle is basically a short 11 blade rolled up into a cylinder, and during groin access without ultrasound imaging, one can shear branch arteries, skewer arteries, dissect plaque, and access too proximally or distally, or into the profunda femoris.
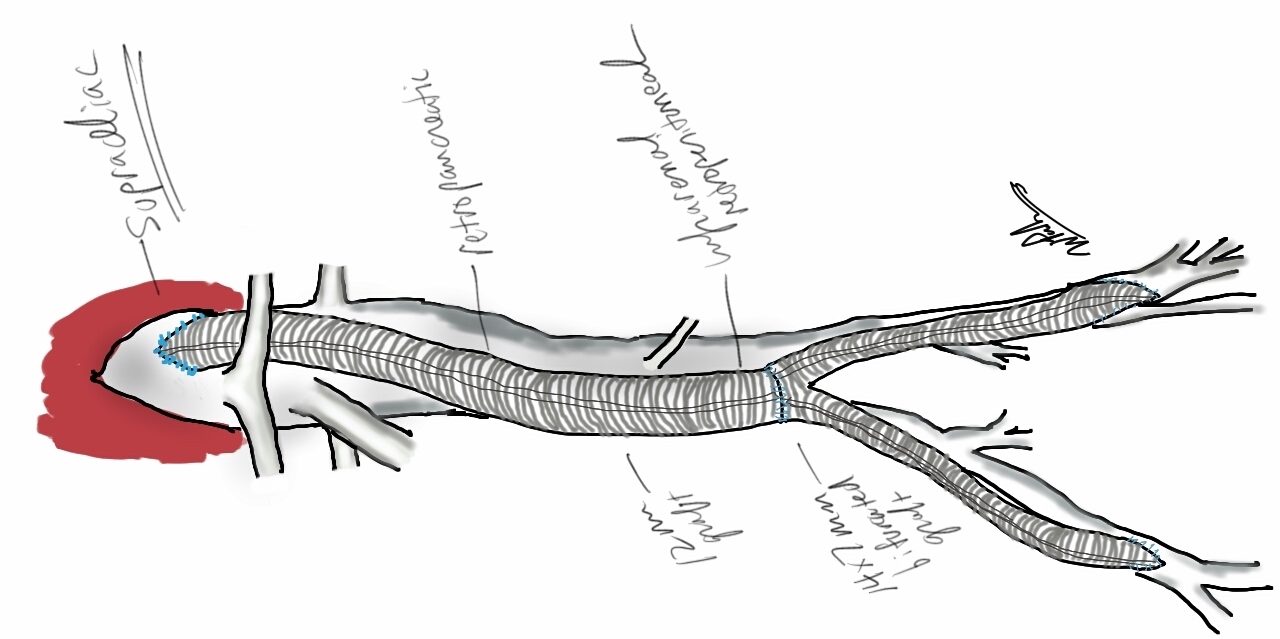
The third need is access to 3D reconstruction software and multislice CTA. This gives you powerful ability to predict which patients are more suitable for a percutaneous approach, and which should have a cut down, and with 3D virtual reality reconstructions, you can plan where the incisions will be. In the skinny patient, this is not a pressing issue, but in the merely obese and the frankly obese, and the super obese, choosing to go percutaneous and avoiding a groin complication, which may be the one thing that debilitates the patient far more than a stent graft deployment, becomes an easy decision with experience.
As you build your 6-8F Perclose experience, you may notice that having too tight and subcutaneous tract can result in the suture catching on SQ fat, and not closing, or that bleeding won’t surface properly and create a hematoma under Scarpa’s fascia, often after the patient gets to the recovery room. Expanding on this principle, as you leap to 12F access and preclosure, I recommend you try this -make a 10mm incision, and using a tonsil clamp, pop through Scarpa’s fascia and seat the tips of the clamp under ultrasound on top of the soft part of the CFA that you intend to access. Gently spreading creates the space that you need to deploy the sutures and ensure that any bleeding will exit the skin and not dive under the fascia. It amounts to an ultrasound guided dissection of the common femoral artery. Before you remove the tonsil, you gently maneuver a micropuncture (always) access needle between the tines of the tonsil clamp until it gets to the artery -this keeps the eventual wire going through the tunnel you just made.
12F can usually close with a single Perclose, but start practicing by placing two Perclose sutures in a 10 oclock and 2 oclock orientation. Once the sutures are in, I make sure the two ends of the suture are pulled out and the end loop of the suture is on the artery and I clamp these sutures to the drapes medially and laterally depending on how I deploy the two sutures. This also helps avoid catching the suture and driving it into the aorta.
After performing EVAR or TEVAR, I remove the sheath, leaving a wire -typically the stiff wire originally supporting the sheath and deploy one of the sutures. This first suture should cinch down onto the artery and substantially decrease the bleeding coming from the access site. I then deploy the second suture, and if the bleeding has stopped or is a steady dribble, I remove the wire. If pulsatile bleeding persists, I recinch the sutures using the knot pushers. If this decreases flow, I remove the wire, otherwise, I place a dilator, stop the bleeding and cut down. Cutting down after SQ dissection means merely dividing skin and tissues over the dilator, and the artery is easily visible for suture placement. If I remove the wire and there is still some bleeding, and usually there is, I place Gel-Foam soaked in diluted thrombin into the tract, reverse heparin, and hold pressure for 10-20minutes. It is very rare to have to convert after this is done.

The skin is closed with an absorbable 4-0 monofilament suture, and skin glue. I usually use the micropuncture needle to give an ilioinguinal field block with Marcaine. This gives 24hrs of pain relief.
A note about incisions. Usually, with 3D VR imaging of CTA, the CFA and its quality (size and absence of plaque), and location relative to the inguinal crease can be ascertained. I try to make the access point at the inguinal crease or distally, as this goes under the subpannus of groin fat rather than through it.

I sincerely believe sheath size is not the limiting factor to percutaneous access. Rather, it is the common femoral and iliac artery. Zakko et al at the University of Florida just published their experience on the obese with percutaneous TEVAR (ref 2), and found that while the arteries were deeper, the technical success rate of staying percutaneous (over 90%) was no different between their obese patients non-obese patients. The predictors of failure were poor access artery quality and size. I believe that you can select for patients most likely to succeed and greatly reduce failure. In this population, groin complications are potentially life threatening, and avoiding an open groin exposure is valuable.
References
1. J Vasc Surg 2012;55:1554-61 (ultrasound guided access)
2. J Vasc Surg 2014;60:921-928 (p-TEVAR and obesity)