
The patient is a younger man in his twenties who began having dizzy spells associated with near syncope and tunnel vision. He was previously an athlete and was fit and never had such episodes -he had a resting heart rate typically in the 60’s or lower. Workup for arrhythmias was ultimately positive for POTS -postural orthostatic tachycardia syndrome and he was referred to Dr. Fredrick Jaeger of our Syncope Clinic. Tilt table testing the demonstrated the reported tachycardia over 140bpm while upright rising from 60bpm while supine. A radionuclide hemodynamic study (Syncope Radionuclide Hemodynamic Test) showed 54% of his blood volume pooled in his left lower extremity and lower abdomen with upright posture. Air plethysmography (PHLEBOTEST) showed abnormal refill and fill times in both legs and a duplex of the legs showed deep venous reflux in both legs. MRV revealed narrowing of left common iliac vein by the overlying right common iliac artery (May-Thurner’s Syndrome, MTS), and this was where the patient came to my clinic.
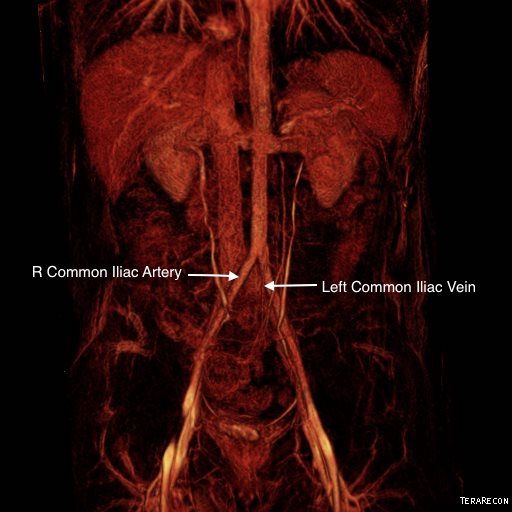
The MRV, shown above and below showed the typical pathoanatomy for MTS, but the patient had no symptoms related to left leg swelling, DVT, or varicosities. He did have a reducible left inguinal hernia which was quite tender.
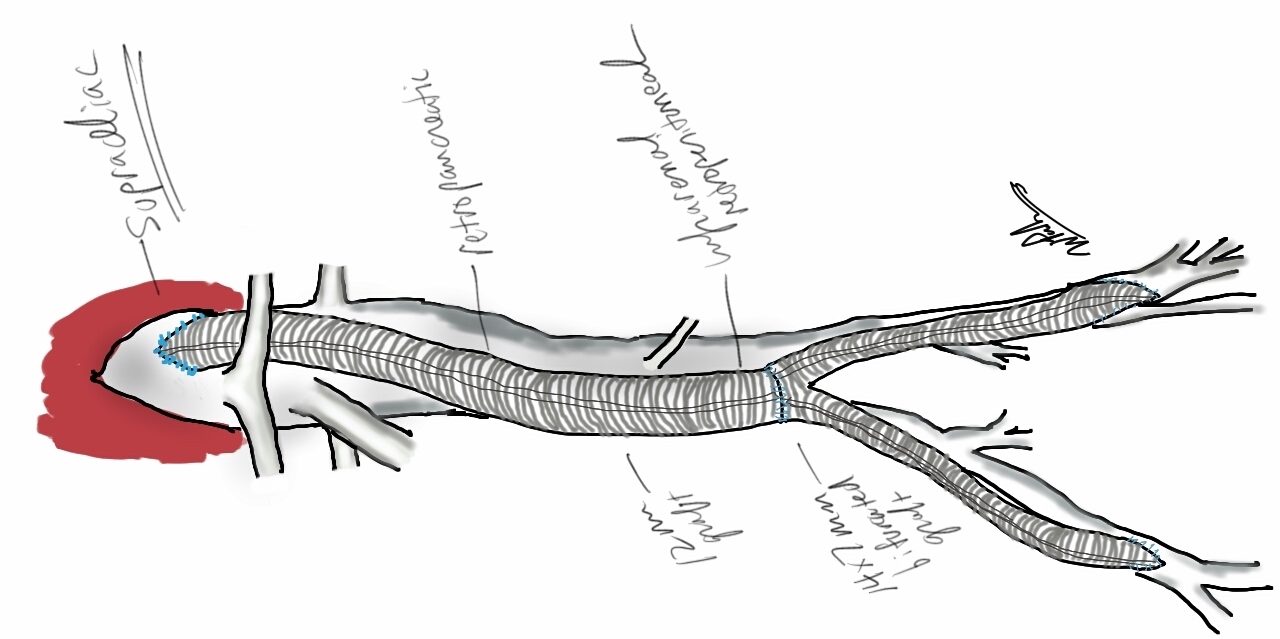
After some deliberation, while not promising anything regarding his POTS, I agreed to proceed with treating his pathoanatomy. Discussion with Dr. Jaeger revealed this: normally about 20% of blood volume parks in the legs with standing which is rapidly dissipated with normal calf muscle pump action. In a subset of patients with POTS, there is a 30-40% maldistribution of blood volume into the legs which may or may not drive the autonomic responses leading to POTS. He has never seen a study result showing a 54% distribution.
It made physiologic and anatomic sense to me to proceed with a venogram and intervention, but I confess I was dubious about any affects I might have on the patient’s POTS and I informed him of it. Also, I recommended seeing a general surgeon for his hernia.
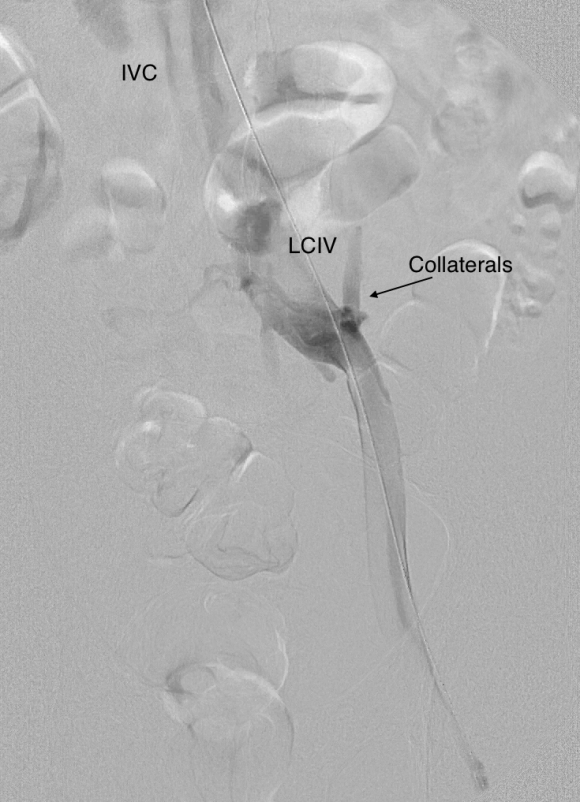
Venography showed obstruction of his left common iliac vein as evidenced by the filling of pelvic and lumbar collateral veins.
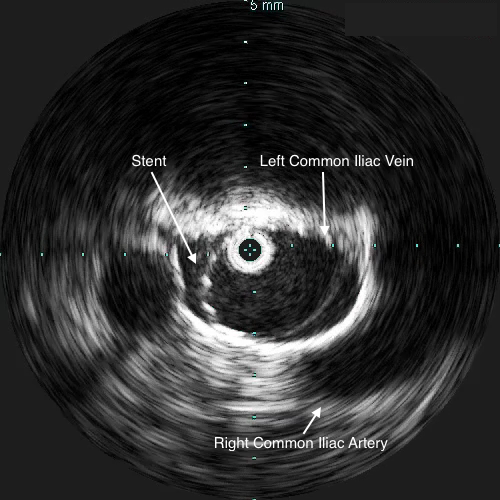
Intravascular ultrasound showed the narrowing better and more directly (panel below). The right common iliac artery narrowed the left common iliac vein severely.

A 22mm Wall Stent was positioned across this and dilated with a 22mm balloon in the IVC and an 18mm balloon in the iliac vein. The resulting venogram showed resolution of the obstruction with collateral veins no longer visualized (below).

But again, IVUS demonstrated more directly the result (and illustrates the importance of having IVUS available for venous interventions).
The patient was discharged after procedure on a baby aspirin only. He subsequently underwent laparoscopic inguinal herniorrhaphy and returned to my clinic about a month later. His followup duplex showed a widely patent stent and normal flows in the left iliac venous system.

Surprisingly -the patient declared that he was cured of his POTS. He said since the stents went in, he has not had any more episodes of near syncope, dizziness, tunnel vision, nor weakness requiring lying down to rest. His wife confirmed that he was a flurry of activity over the holidays that was surprising considering how debilitated he was before. This is astonishing to me.
But it should not be a surprise given this: if the POTS symptoms were the result of autonomic dysregulation, a breakdown of the feedback control loop, there were only several places this could be a problem.

The pathology, the MTS, explains the POTS in this instance very nicely. Because the problem was in the cardiovascular system part of the diagram which I can fix and not the autonomic nervous system control element, which I can’t fix yet, a solution could be tried. This was not an asymptomatic compression of the iliac vein which we do encounter as an incidental finding. It seems to be POTS caused by MTS, and cured for now by treatment of the MTS.
18 replies on “POTS+May-Thurner’s Syndrome: Rare Disease Causes Rare Disease?”
My daughter has elers danlos syndrome III + pots.
Her IVC vein is pretty well collapsed. She has not responded to medications due to medication sensitivity. She has responded to iv fluids. She has had 2 different ports for receiving fluids however this last one has to come out. She cannot get another one in the near future. My question.. I have suggested several times that we try a Stent to keep the vein open but was told IVC veins are too small and delicate for a stent.
What is your opinion on stent and the IVC?
LikeLike
The POTS is tenacious. We are tracking two patients who initially responded to stenting but one was going to be investigated for symptom recurrence -i had left US at that point and will be publishing on this. ED and POTS being related is some kind of clue but not having a good theory of he disease is a handicap. These venous stents will close unless they are generously sized. In a child, I would hesitate. Contact me through email by calling my office at Cleveland Clinic 216 444 6268
LikeLike
I was diagnosed with POTS but I have tight heavy mid abdominal pain 24/7 in all positions. I must wear ab binder to function. Please help me. Can I send you a CD of my CT scan and MRI for second opinion?
LikeLike
My husband healthy 41 year old got diagnosed with POTS and May Thurner’s Disease within weeks of eachother from 2 different heart doctors. He just got a stent put in because his vein was completely closed his leg was so swollen he couldn’t walk on it and was so painful. He is in a lot of pain now in his back from the surgery even through they went through his groin . I’m hoping he was misdiagnosed for this then will help him so much that he doesn’t notice the POTS symptoms. Glad to have found this article.
LikeLike
Hello Mrs. Conger -the stents typically cause inflammation in surrounding tissues. In a left iliac vein to vena cava stent this causes inflammation on the lumbar spine and under the aortic bifurcation. Typically this is self limited and can be managed with anti inflammatory medications. Would love follow up as to your husband’s POTS symptoms.
LikeLike
I am a 41 year old female with POTS and MTS. Since as long as I can remember every time I get up My vision goes black, I get dizzy and have to lower my head so that I don’t pass out. I found out about the MTS when I developed a 4Ft long blood clot in my left leg up to my diaphragm. I had 100% blockage of my CIV. My blood clot had to be sucked out during fluoroscopy and the stent placement was very difficult because of the obstruction. Last year I went to a vascular md and he determined that even after stent placement I continue to have high blood pressure in my legs and extremely low in my upper extremities. I took a job at a factory and because my leg muscles were not contracting I started having fainting spells at work. I never passed completely out. It was more like I couldn’t keep my eyes open and head up. At first I thought I wasn’t getting enough sleep but increased sleep did not improve my symptoms. As a matter of fact after working standing up and still for 3 months, I could no longer stay completely conscience. My supervisor made me take a drug test, lol, which was negative. I’m ALWAYS TIRED now! My left leg is still larger than my right. I just haven’t had another clot since my stent. I am a registered nurse and I believe my symptoms are permeant due to damage done to my veins in my legs due to the obstruction and constant high pressure. I believe my leg veins have been stretched out and have lost their ability to contract so that blood is forced upward. I believe that the longer I worked at that factory job, the more blood collected in my legs and the high pressure dilated the veins more everyday. Then after 3 months my heart simply wasn’t able to pump enough oxygen rich blood to my brain thus the feeling like I cant stay awake but really I was passing out. I could feel the firmness in my legs from too much blood. Once I laid around for a couple of days the firmness went away. this is my number 903-819-7957. I’m Kimberly!
LikeLike
A blood pool study (a nuclear medicine diagnostic scan) might show pathologic swelling of blood volume as well as an ascending venogram
LikeLike
I am a 29 y/o female with Pelvic Congestion Syndrome and now, as it seems, POTS. I’ll back track a little bit and hope that you can help me make some sense of this. I had no issues/POTS symptoms before left ovarian vein embolization for PCS. The embo resolved my pelvic pain/low back pain issue that was the primary reason for seeking treatment. I have no children so we still are unsure how/why I ended up with PCS and a completely refluxing left ovarian vein. Did venogram with IVUS to check for compressions before embo… and I was told both the renal and iliacs were fine…
Ever since my embolization I have been experiencing issues with my heart rate/blood pressure so I’m doing the workup with a pending diagnosis of dysautonomia according to my physician. I guess my question is, why? Is there the possibility of a missed compression/MTS? Is that a common thing to miss? I’m extremely frustrated with the medical system right now (I’m a sonographer working for Cleveland Clinic Florida) because I can’t get any answers. My normal resting heart rate and BP were perfectly fine before this embolization. I exercised often, even working as a personal trainer on the weekends. I went from athletic and active all the time, to being stuck on the couch. I’ve tried everything that has been thrown my way, and no consistent relief and no one wants to help me dig deeper for any answers. Now, I can have a normal resting heart rate and I feel the change to the 120s and above by simply standing. And this blood pressure issue is through the roof. I have hypertensive episodes after any somewhat strenuous activity (123-130/100 and above) with narrow pulse pressures, that are only relived by sitting or lying down, or lying down with my feet over my head braced against the wall. Venous reflux study showed insufficiency in both the superficial and deep system still even after embo but I’m being told that alone isn’t severe enough to cause this blood pooling. As soon as I stand up, my legs, especially my left, begin to discolor and mottle. It is driving me crazy. My left one especially does this. Wearing 20-30mmhg thigh highs just to keep somewhat functional and they help most of the time with the swelling, but not with this crazy heart rate and BP. I’ve been to both an IVR and a Cardiologist and both just keep going back and forth saying it’s the other person’s issue…and I’m still sitting here with both problems now 😦 I feel like I should have just left myself with the pelvic pain with all that this has caused now. Could this be missed MTS? Is there anything I can do, or am I just out of luck? It is extremely frustrating and I apologize for rattling on… I’m just looking for any answer that could give me even some of my life back and came across your page.
LikeLike
I’m sorry to hear this. Send me an email. I still have my clinic email.
LikeLike
Hi Dr. Park,
What is your email address?
Thank you!
LikeLike
Follow me on Instagram -docpark and DM me
LikeLike
Ok, I sent a message to your instagram. Thank you doctor!
LikeLike
Dr. Park,
I am a 32 yo male with pots and ehlers-danlos. I recently had a venogram and intravascular ultrasound. Can I contact you with additional information? I do not have Instagram. Is there another way to reach you?
LikeLike
Direct message me @docpark on Twitter or call answering service 440.333.8600
LikeLike
I have POTS and was told by a doctor doing my EMG that I need to be seen by a vascular doctor. The last one I seen didn’t even know what POTS was and didn’t do any tests to figure out why my feet turn purple. I can’t help but think I might have something like this causing my POTS. Are you still practicing in Ohio?
LikeLike
Yes I am at University Hospitals in Cleveland.
LikeLike
My now 17 year old daughter developed POTS after a Covid infection in 2020. I did as well (46). She recently was diagnosed with MTS and underwent a stent procedure. As in your article, her POTS symptoms were immediately non existent and continue to be. Our vascular doctor suspects I have the same issue and I will be undergoing the venogram soon. But according to our POTS specialist, pots patients with MTS who undergo stenting, 70% recover from pots. There is most definitely a link and I have been able to find studies showing this as well. Like you, our vascular doctor was very hesitant to say it would help the pots simply because it’s not a guarantee. But he sees it in his practice all the time because our POTS doctor refers his patients to him so he works with a lot of those people.
LikeLiked by 1 person
I agree. Need these cases collected and published and subject to peer review. The variable course of POTS is such that a sure promise is not possible but certainly there are physicians and surgeons willing to take on this terrible condition which is a start.
LikeLike